
In a large clinical trial assessing Apretude, ViiV Healthcare’s recently approved injectable drug, as a form of HIV prevention, seven participants contracted the virus despite receiving their injections on schedule.
The new findings indicate that, just as with those who take daily pills to prevent HIV, breakthrough infections are possible among people receiving Apretude.
Dr. Raphael J. Landovitz, who led the Apretude clinical trial in question, told NBC News that he expects such cases of PrEP failure to remain what he characterized as rare, regardless of which form of preventive antiretroviral medication people at risk of HIV receive.
Apretude is nevertheless so efficacious, Landovitz said, that the drug has “the potential to end the HIV epidemic, particularly for people who are challenged with taking oral PrEP.”
Landovitz, an infectious disease specialist at UCLA, said it might always remain unclear why the breakthrough infections among those receiving Apretude occurred. He and his colleagues already know that the blood concentrations of the drug in the first four people to experience such infections weren’t unexpectedly low.
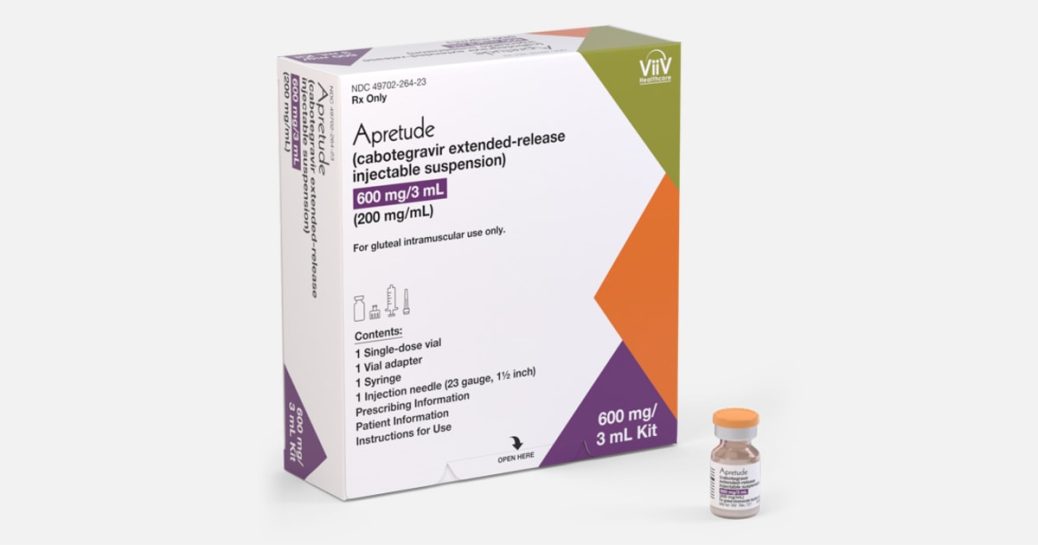
The Food and Drug Administration approved Apretude for use as what’s known as pre-exposure prophylaxis, or PrEP, against HIV on Dec. 20. The long-acting drug, which is meant to be injected every two months by a health care worker, joined two daily pills — Gilead Sciences’ Truvada and Descovy — that were approved as PrEP in 2012 and 2019, respectively.
When taken daily, oral PrEP reduces the risk of contracting HIV by 99 percent or more among men who have sex with men, or MSM — the group that comprises the vast majority of PrEP users.
But many people at risk of HIV are disinclined to remain faithful to such a daily-pill regimen — in particular, research has indicated, Black MSM. This demographic has the nation’s highest rate of new HIV cases, but has long lagged behind its white counterparts in both starting and sticking with PrEP.
HIV advocates have looked to Apretude as a potential solution to this enduring medication-adherence problem. And yet, receiving Apretude requires a clinic visit every two months, compared with visits every three months to maintain a prescription to Descovy or Truvada as PrEP.
Men who have sex with men account for an estimated 70 percent of the approximately 35,000 HIV transmissions in the United States each year, according to the Centers for Disease Control and Prevention.
Apretude vs. Truvada
One of the two double-blinded clinical trials that prompted the FDA to approve Apretude for use as PrEP included 4,566 cisgender MSM and transgender women in the U.S. and six other nations in Latin America, Asia and Africa. (A second trial included cisgender women in Africa.) Half of the 1,698 U.S. study members were Black.
The participants, who were all deemed at substantial risk of contracting HIV, were randomized to receive Truvada or Apretude, with each group receiving a corresponding placebo.
In 2020, Landovitz and his colleagues announced that after a median of about 17 months of follow-up during the study’s blinded phase, those who received Apretude had about a two-thirds lower HIV acquisition rate compared with those who got Truvada. This stark difference was driven by suboptimal adherence to the daily Truvada regimen and, by comparison, greater Apretude coverage of the participants’ sex acts.
On Tuesday, Landovitz presented updated trial findings at the virtually held Conference on Retroviruses and Opportunistic Infections He reviewed data from the 12 months following the study’s mid-2020 unblinding.
During that period, the rate of new HIV cases rose in both the Apretude and Truvada groups. This phenomenon, Landovitz suggested, was likely driven by two factors. Firstly, participants’ adherence to both the injection schedule and the pill regimen was lower after the unblinding. Additionally, during this latter trial phase, a greater proportion of the participants were living in Latin America, where the background HIV transmission rates were relatively high.
Nevertheless, Apretude injections maintained about the same rate of superior overall protection against HIV compared with oral PrEP as seen during the trial’s blinded period.
During the combined study periods, 25 people in the Apretude group and 72 people in the Truvada group contracted HIV during a nearly identical amount of cumulative follow-up time.
Breakthrough cases
The seven breakthrough infections among people who received their injections on schedule occurred during a cumulative 4,660 years of follow-up among all those in the Apretude arm of the trial. (During that time, an additional 18 people contracted HIV who did not receive Apretude on schedule.) This means that if a group of 10,000 people in similar circumstances were given Apretude, about 15 of them would be expected to experience breakthrough HIV infections over one year.
The first case of PrEP failure among an individual adhering well to a daily-pill regimen was reported in 2016. Since then, there have been a handful of additional reported cases, which have largely been the apparent result of people contracting relatively rare HIV strains that are resistant to the pair of antiretrovirals, tenofovir and emtricitabine, that are included in both Truvada and Descovy.
Transmission of HIV that is resistant to Apretude’s antiretroviral class, Landovitz said, is “vanishingly rare.” So he said that drug resistance cannot explain breakthrough infections among those receiving the injectable as PrEP.
Breakthrough infections also occurred in at least one, possibly two, people in the Truvada group of the Apretude trial including trans women and MSM. One additional such breakthrough case occurred in the corresponding trial of cisgender women. Further analyses are needed to determine if after each trial’s unblinding, additional people contracted HIV while adhering well to the Truvada regimen.
Research has indicated that compared with concentrations of Apretude in the blood, concentrations of the drug are about 90 percent to 92 percent lower in rectal tissues but only about 80 percent lower in tissues in the vagina and on the cervix. Landovitz told NBC News that these disparities could possibly help explain the emergence of the seven breakthrough infections among those in the Apretude arm of the PrEP study including trans women and MSM. So far, ViiV is able to report that in the PrEP trial including cisgender women, there were no cases of Apretude failure during its blinded phase; further analysis is needed to determine if such breakthrough infections occurred after that study’s unblinding.
Cost and availability
Apretude is not yet widely available in the United States. ViiV is campaigning for insurers to add the injectable preventive to their lists of covered medications.
The pharmaceutical company is up against the fact that multiple generic versions of Truvada hit the market last year and now cost as little as $26 per month. Apretude is priced at the equivalent of $1,850 per 30-day period, similar to Gilead’s pricing of Descovy and brand-name Truvada. The CDC reported at this week’s retrovirus conference that during the first three quarters of 2021, about 42 percent of U.S. PrEP prescriptions were for generic Truvada.
In a paper that Landovitz wrote with Dr. Anne M. Neilan of Harvard Medical School and others and published in the Annals of Internal Medicine on Feb. 1, they conclude that Apretude would need to have a monthly cost no greater than $308 over generic Truvada’s price to remain cost-effective.
Due to the U.S. Preventive Services Task Force granting it an “A” rating in 2019, oral PrEP must now be covered by almost all private insurers with no cost sharing. That means both the medication and the quarterly clinic visits should be free to people with private health plans. Medicaid and Medicare also cover pill-form PrEP, but they may still demand out-of-pocket payments for the prescription.
Carl Schmid, executive director of the HIV+Hepatitis Policy Institute in Washington, reported that advocates such as himself have been pushing the task force to swiftly include Apretude in PrEP’s “A” grade.
In the meantime, ViiV will offer a copay card to people with private insurance that will cover up to $7,500 in out-of-pocket expenses related to the injectable drug each calendar year, plus $350 toward injection-administration fees.
Dr. Rupa R. Patel, the PrEP Clinic Lead at Whitman-Walker Health in Washington, told NBC News that Apretude’s considerable efficaciousness notwithstanding, the drug’s every-other-month dosing schedule “is still not ideal.”
“Something taken every six months or 12 months would be better, of course,” he said.
Multiple additional forms of long-acting PrEP, dosed as seldom as twice per year, are indeed in the pharmaceutical pipeline. However, Merck announced in December that the company was putting a hold on all clinical development of its experimental drug islatravir after the long-acting antiretroviral was linked to declines in some trial participants’ CD4 immune cells — white blood cells that provide a key indication of immune health. This trend occurred both among those receiving the drug as HIV treatment and in those receiving it as PrEP.









Recent Comments