Recognizing that giving Covid-19 booster shots every few months is not a feasible public health strategy, the Food and Drug Administration convened its panel of outside advisers Wednesday to plot out a framework for how to approach future doses of the vaccines.
The FDA sought guidance from the Vaccines and Related Biological Products Advisory Committee about what sorts of updates the vaccines may need before a potential winter surge in cases.
Full coverage of the Covid-19 pandemic
But the committee members were presented with an extremely short timeline: Dr. Peter Marks, the FDA’s top vaccine regulator, told the panel that scientists would need to determine which strain or strains to target by May or June, so drugmakers have enough time to produce the shots by the fall.
The resulting discussion had moments of exasperation, as committee members complained of a lack of information needed to make such decisions, as well as a lack of clarity about what, specifically, the FDA was asking of them.
Ultimately, the panel of vaccine experts were unable to come up with a plan, saying there were a significant number of unknowns, including what strain of the virus the world may be dealing with in the fall and what level of protection was warranted.
“I think we’re looking at a conundrum here,” Dr. Ofer Levy, the director of the Precision Vaccines Program at Boston Children’s Hospital, told his colleagues.
The FDA said more meetings would be held on the issue before any decisions were made.
The Covid vaccination schedule in the U.S. has so far been determined in real time, with federal regulators often looking to other countries, such as Israel, for data about when to authorize new shots.
With the FDA’s recent authorization of second Covid booster shots for older adults, the strategy has come under scrutiny. Health experts have argued that it is not practical for people to get an additional shot every four months.
What level of protection?
Also of concern is whether a new variant emerges that renders the current vaccines less effective. The BA.2 omicron subvariant — currently dominant in the U.S. — already deals a significant blow to the existing vaccines.
Even so, the mRNA vaccines from Moderna and Pfizer-BioNTech currently being given in the U.S. still protect against hospitalization and death.
Panel members wanted to know what kind of protection they should expect the Covid vaccines to provide — is there a current threshold of effectiveness below which new vaccines are needed?
Scientists have not yet established so-called correlates of protection, which are immunological markers that can be used to predict the level of effectiveness a vaccine may provide.
What is considered “insufficient protection?” committee member Dr. Cody Meissner, a pediatrician at Tufts University School of Medicine, asked. “Since we don’t know the correlates of immunity, we’re going to be dependent on hospitalization rates and death rates.”
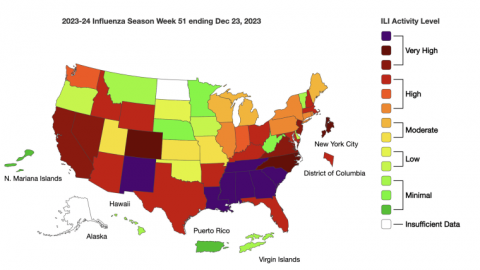
A flu shot approach
Marks of the FDA suggested an approach similar to how the flu shot is made each year, in which World Health Organization scientists constantly monitor influenza strains and, every year, select three to four that they think will be circulating widely to include in the flu vaccine.
Some committee members, however, rejected the idea that Covid vaccines could be approached in the same manner as the flu.
Earlier in the day, Trevor Bedford, a computational biologist at the Fred Hutchinson Cancer Research Center in Seattle, presented data to the committee that showed the coronavirus has been evolving more rapidly than influenza.
A committee member, Dr. Hayley Altman-Gans, a pediatrician and infectious disease expert at Stanford University Medical Center, also noted that the coronavirus has not always followed the same seasonal pattern as influenza.
What kind of Covid vaccine?
It was agreed that the next Covid vaccine should target more than one variant and that all vaccine makers should formulate the doses to include the same variants.
Deploying a vaccine that targets more than one variant, also known as a multivalent vaccine, could provide broader protection than the existing vaccines.
Moderna has said it is developing a vaccine that targets both the delta and the omicron variants that could be ready by the fall.
“I think that we need to use our predictive models and perhaps pivot to a multivalent approach,” said a committee member, Dr. Michael Nelson, the chief of the asthma, allergy and immunology division at UVA Health in Virginia.
Throughout the pandemic, vaccine makers have decided what strains to include in clinical trials. Although they have tested versions of the vaccines specific to certain variants, no company has moved ahead to deploy the shots, instead continuing to use the vaccines made for the original strain of the coronavirus.
But the committee largely agreed that the variants to target should come from an official source, not the drugmakers on their own.
“It shouldn’t come from them,” said a committee member, Dr. Paul Offit, a vaccine expert at Children’s Hospital of Philadelphia. “It should come from us.”
Follow NBC HEALTH on Twitter & Facebook.







Recent Comments