A full two years into the coronavirus pandemic, long-haul Covid patients remain sick and in desperate search of answers. They’ve lost jobs. They’ve lost their sense of self. Many say they have lost faith in the medical community.
Despite multiple studies, the launch of dozens of specialized long Covid clinics and $1.15 billion in federal funding for the National Institutes of Health to study the condition, there remains a dearth of proven treatments for people who are suffering from lingering illness after their infection.
Full coverage of the Covid-19 pandemic
“There is no one right answer for many of our patients,” said Dr. Ben Abramoff, director of the Post-COVID Assessment and Recovery Clinic at Penn Medicine, which has seen more than 1,100 long Covid patients.
Compounding the problem is a lack of consensus on how to define long Covid, according to a commentary published Tuesday in the Annals of Internal Medicine from researchers at UCLA Health and the David Geffen School of Medicine in Los Angeles.
“We do not know what constitutes long Covid or how to formally diagnose it,” the authors wrote. “An improved understanding of this condition is needed to provide appropriate care for our patients.”
Most hospital-affiliated clinics, including Penn Medicine, treat patients with a variety of medical teams, including counselors, cardiologists, pulmonologists, physical therapists and immunologists.
But it can take months to get an appointment, and many patients say finding treatment for long Covid can be time-consuming and draining. That gap has allowed private companies to step in with promises of relief.
The most well-known is IncellDx, a California-based company that said it has accomplished three key goals specific to long Covid: a diagnostic test, a treatment plan, including an HIV drug and cholesterol-lowering medications, and a way to show patients that the treatment is working.
Critics counter that there are no simple blood tests or widely accepted biomarkers to determine whether someone has long Covid. Even at highly respected clinics, treatment regimens vary widely and doctors don’t offer cures. Instead, most treat the symptoms in an effort to get patients back to some sense of normalcy.
The myriad symptoms that come with long Covid make it difficult to come up with a standardized treatment.
The illness, characterized by lingering symptoms weeks to months after an infection, can take on many forms. Some people have daily migraines. Others lose their train of thought midsentence. Some can no longer walk the short distance from their front door to their mailbox.
Long waits and long-term plans
In the past two years, scores of long Covid treatment clinics, typically affiliated with hospitals or medical research centers, have opened nationwide.
When Laurie Bedell, 42, of Pittsburgh, first sought treatment, she waited nearly eight months for an appointment at the Cleveland Clinic more than 130 miles away. When her health insurance refused to pay for the visit, she was forced to find a doctor closer to home.
“I waited months and got nothing done,” she said. “I’ll probably be waiting months again for hopefully somebody in Pittsburgh.”
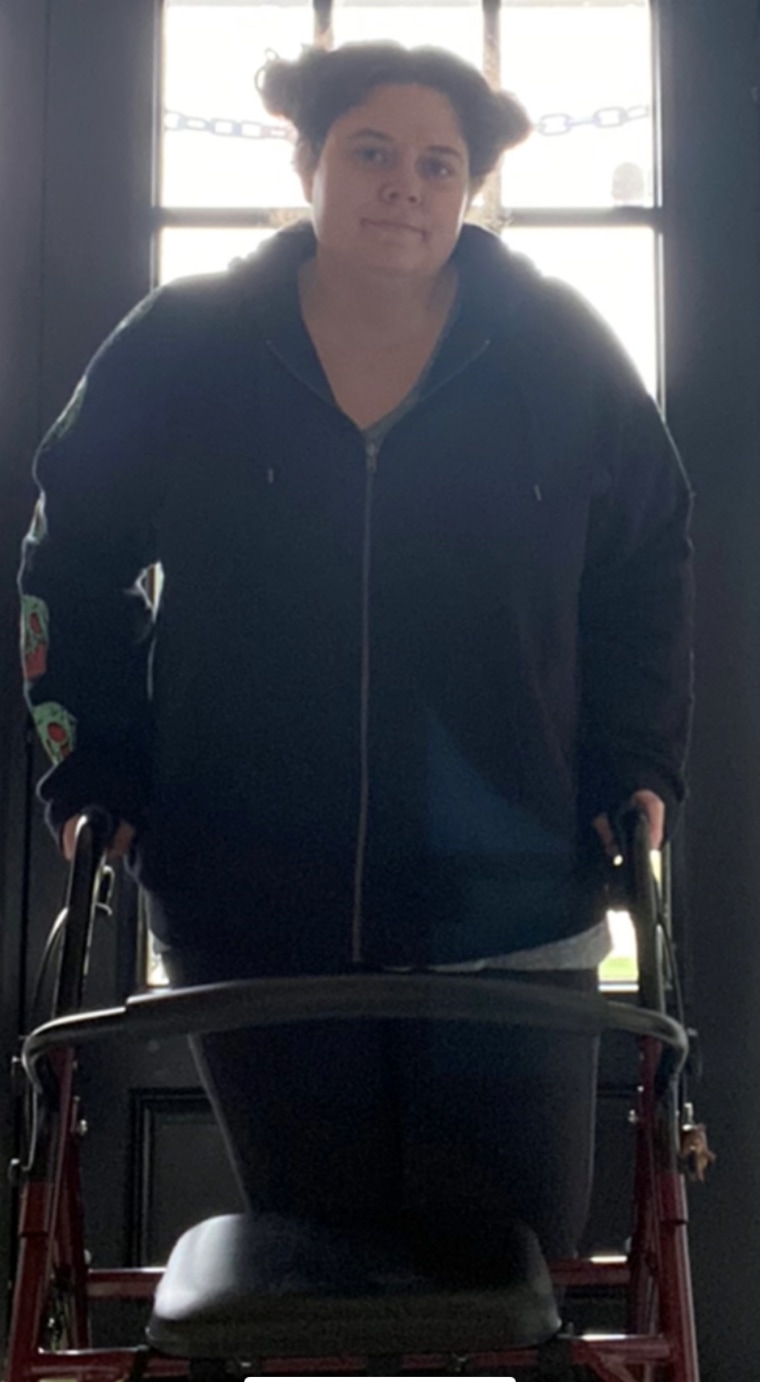
The wait is not easy for patients like Bedell — a former nursing director who, before Covid, was accustomed to working out for two hours, six days a week. Now, she said, “I physically can’t function. I have a walker. I can’t drive because I have cognitive dysfunction, and my vision’s constantly blurry.”
At the Covid Activity Rehabilitation Program at the Mayo Clinic in Rochester, Minnesota, where doctors have treated hundreds of people with long Covid, patients are advised to take their recovery slowly.
“Patients, when they get sick, they just so want to get back to normal life,” said Dr. Greg Vanichkachorn, an occupational medicine specialist who heads Mayo’s post-Covid program.
But plunging into normal activities is exhausting after so much time being sick, and can lead to flare-ups and fatigue that feel like a relapse.
“The body just can’t handle that,” he said. “Pacing is so important — helping people understand the importance of proper pacing from the very get-go so they don’t get into this situation.”
Vanichkachorn, like many long Covid clinicians, focuses on treating symptoms. He often prescribes a blood pressure medicine called midodrine and a steroid called florinef in an attempt to improve blood flow in the body. Physical therapy is also important, he said, to help keep muscles toned and as strong as possible.
Hinda Stockstill, 35, of Cincinnati, said her long Covid has improved following a combination of treatments from both her family doctor and physicians at the Cleveland Clinic’s post-Covid treatment center.

She has undergone physical and occupational therapy, and has taken an antiviral called acyclovir and fluvoxamine, which treats depression.
“It didn’t cure me completely,” Stockstill said. “I still do have some days where I’m just so tired, I can barely get up. But they’re fewer and far between.”
“Most patients have improvement over time,” Abramoff said. But about half “don’t get back to 100 percent.”
No answers yet at the NIH
The cause of long Covid is still unknown. Why do some people infected with the coronavirus recover, while others continue to be plagued by symptoms?
Several theories exist. A recent study suggested that the immune systems in some people do not react appropriately to the virus, and don’t trigger the correct antibodies. Another study found that the coronavirus may reactivate the Epstein-Barr virus, which causes mononucleosis, or be linked to Type 2 diabetes.
In February 2021, the NIH energized legions of long-haulers with the allocation of more than $1 billion for long Covid research through 2025.
We all were really hopeful — like, OK, finally something is happening!
“We all were really hopeful — like, OK, finally something is happening!” Bedell said. She was part of a focus group of long Covid patients from which the NIH sought guidance as it began its flagship research project called Researching COVID to Enhance Recovery, or RECOVER.
The research aims to enroll 20,000 people. As of Friday, 1,175 had been enrolled, a prime example of how painstakingly slow the scientific process can be — even during a pandemic.
“I understand people are desperate,” said Dr. Stuart Katz, a principal investigator of the RECOVER trial, as well as the director of New York University Langone’s heart failure program.
The goal of the trial is not to treat patients, at least not at first.
“We’re trying to define, ‘What is long Covid? What are the best diagnostic tools?'” he said.
If potential treatments are recommended, it’ll be after researchers have scoured “the entire scientific literature,” Katz said.
“It’s a huge undertaking, but if we’re going to ask sick people to be in a study and devote resources to that study, we want to try to offer the best, most promising treatment,” he said.
A test for long Covid?
For some patients, the long waits, the lack of clear answers and the slow steps toward recovery are too much to bear. That’s why thousands have turned to IncellDx, a diagnostic company based in San Carlos, California.

After months of dizziness, shortness of breath and nerve pain, Sara Anaya, 43, of Santa Maria, California, went to the Covid Recovery Clinic at Keck Medicine of the University of Southern California, where she said she was offered physical therapy, mental health counseling and neurological testing.
She tried the physical therapy, but said it left her even more fatigued to the point where she could not get out of bed for days. She was frustrated, she said, that the USC clinic would not offer medications, even though none has been approved to treat long Covid.
“A lot of people think what they want is a pill,” Abramoff, of Penn Medicine, said. But “we don’t have that pill, and we’re not particularly close to having it.”
A lot of people think what they want is a pill. We don’t have that pill, and we’re not particularly close to having it.
Anaya turned to IncellDx, where she was able to get a telemedicine appointment with the company’s founder, Dr. Bruce Patterson, “almost immediately.” All patients are seen virtually.
Patterson is a virologist who was heavily involved in HIV research for decades before shifting his focus to long Covid in 2020.
The main premise of IncellDx is a diagnostic blood test which the company claims can diagnose long Covid, help determine effective therapies and show any improvements after treatment. IncellDx does not do blood draws; instead, patients must send a blood sample to the company for analysis.
The test looks at levels of 14 immune system proteins called cytokines that the company says indicate the blood vessel inflammation specific to long Covid.
Those 14 markers were identified using mathematical modeling and artificial intelligence, Patterson said. They’re able to show, he said, “what’s different about these long Covid patients?”
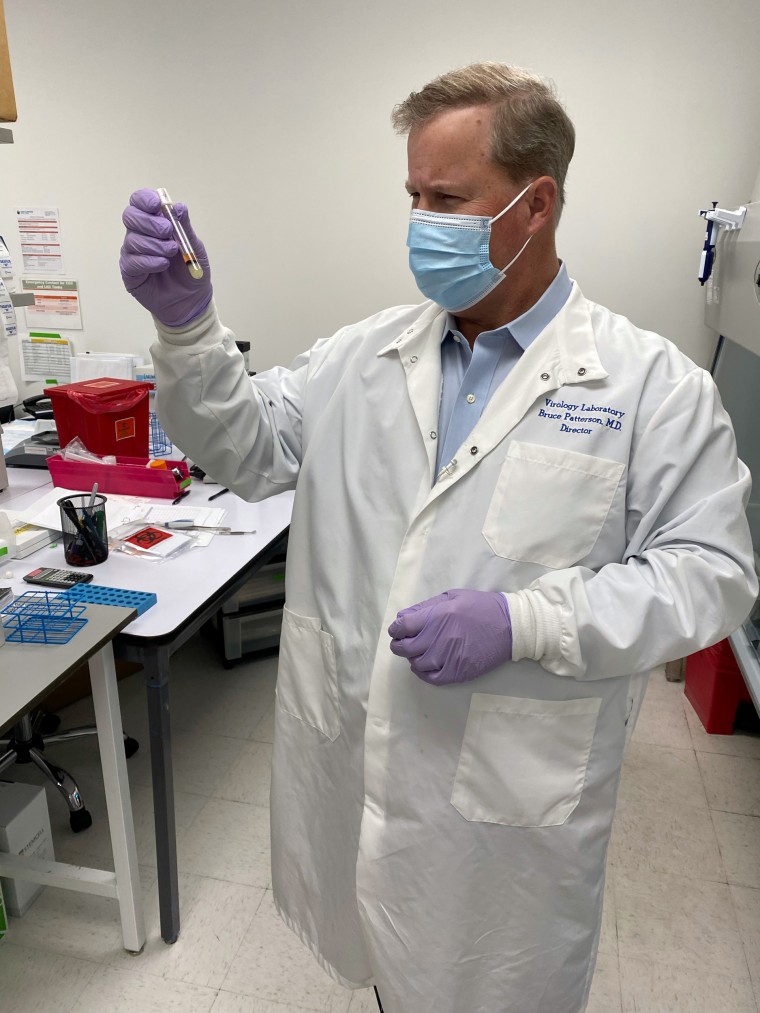
IncellDx clinicians don’t prescribe drugs directly to patients, but do provide patients with a “treatment recommendation” that they can take to their personal physicians. It typically includes an HIV drug called maraviroc, and statins, which are usually used to lower cholesterol. Neither are approved to treat long Covid.
Long Covid physicians affiliated with hospitals and major medical centers dispute whether the diagnostic test is valid. While some clinics do blood tests and imaging to learn more about what’s going on in a patient’s body, nearly all rely on symptoms to make a diagnosis.
“You don’t need a blood test to diagnose long-haulers,” said Dr. Kanao Otsu, lead immunologist at the Center for Post-Covid Care and Recovery at National Jewish Health in Denver. “You don’t need a cytokine panel to tell you that you’re still suffering from your Covid that you had nine months ago.”
More than 18,000 people have taken IncellDx’s test, Patterson said. Nearly all — 95 percent — have been diagnosed with long Covid based on it.
Download the NBC News app for full coverage of the Covid-19 pandemic
That’s a red flag, said Dr. Marc Sala, a pulmonologist and critical care specialist who sees long Covid patients at Northwestern Medicine’s Comprehensive Covid-19 Center. A test can only be validated, he said, through using it on a diverse group of people — in other words, a large mix of people both with and without long Covid.
What’s more, there is no evidence to prove that raising or lowering any of IncellDx’s long Covid markers can actually treat the condition, he said.
“None of this is based on human trial data,” he said.
Patterson said the company plans to carry out randomized clinical trials, but defended moving forward without them in the meantime.
“We’re in a pandemic,” he said. “I don’t know that these patients can wait 18 months for the results of a trial.”
Anaya said the medications recommended by IncellDx and prescribed to her by a local doctor worked, though it took a couple of months. She still has very little sense of smell.
Not all patients have had similar success.
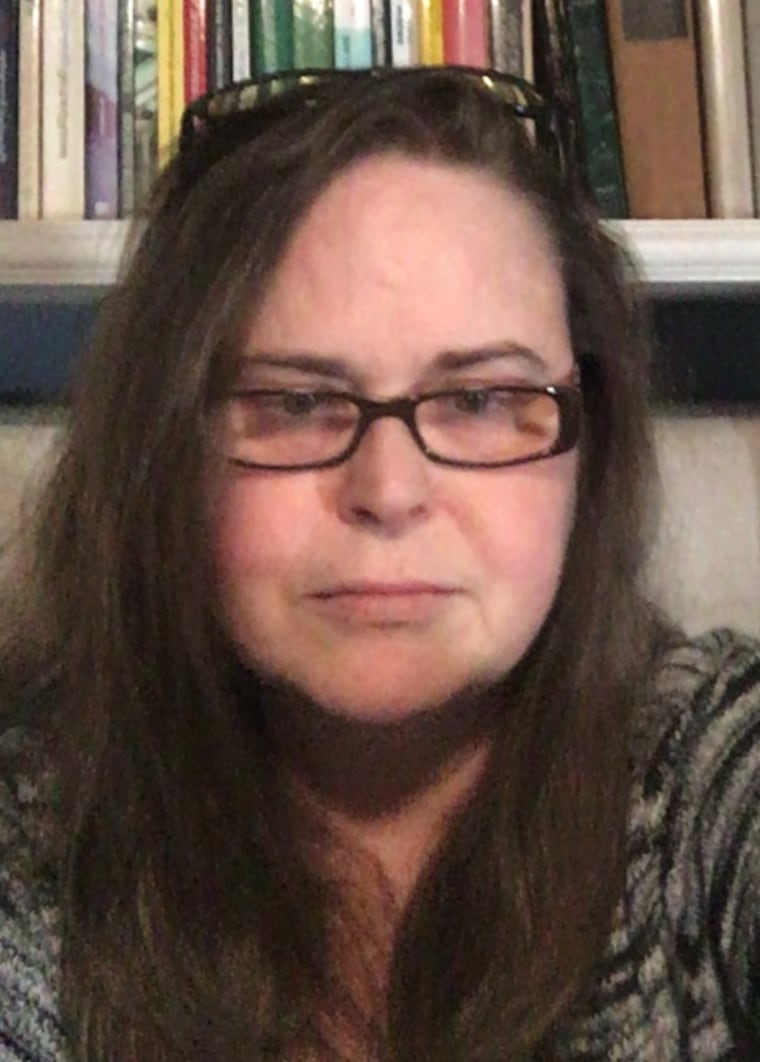
Anne McCloskey, 53, of Seattle, was part of the IncellDx’s original research and was not charged any fee when she sought help in November 2020.
IncellDx’s tests showed that she had elevated levels of biomarkers that indicated long Covid. She started with the company’s regimen, along with several other treatments.
Several months later, a repeat IncellDx blood test suggested she’d largely recovered. But McCloskey still suffered from fevers, extreme fatigue and memory lapses.
[Patterson] told me that I was his poster child for recovery. And I’m like, you know, I’m still really sick.
“[Patterson] told me that I was his poster child for recovery. And I’m like, you know, I’m still really sick.”
The extreme vulnerability of long Covid patients makes it all the more important for doctors — in clinics and companies — to avoid making promises that a test or treatment is the definitive answer without rigorous scientific study and data to back them up, said Dr. Myles Sheehan, director of the Pellegrino Center for Clinical Bioethics at the Georgetown University Medical Center.
The danger, he said, “is that the hope that they offer will be proven false, which could be very devastating to people who are reaching out like a drowning man asking for somebody to save him.”
It is that lack of scientific data that makes already vulnerable long Covid patients even more susceptible to unproven claims, said Dr. Ziyad Al-Aly, a clinical epidemiologist and long Covid researcher at Washington University in St. Louis.
“I worry that our collective inability to put together trials to come up with therapeutics for these patients with long Covid creates the opportunity for other groups and companies to exploit patients,” he said.
“We are dropping the ball on long Covid patients.”
Follow NBC HEALTH on Twitter & Facebook.








Recent Comments